Epidermal Inclusion Cyst
|
|
Time to read 10 min
|
|
Time to read 10 min
In my dermatology practice, one of the most common skin conditions I see are epidermal inclusion cysts,(also called blind pimple, acne nodules, acne cysts or sebaceous cysts). These hard bumps under the skin can be frustrating and painful, so I want to provide some guidance on how to identify, prevent, and treat these pesky cysts.
Not all acne nodules are cysts, but the ones that last months and won't go away are usually cysts.
If you get a lot of cysts, you are not using the best skin care routine for your skin type. There are 16 Baumann Skin Types. Take the skin care routine quiz and we can help you build a skin care routine to prevent cysts.
[[ctaquiz]]
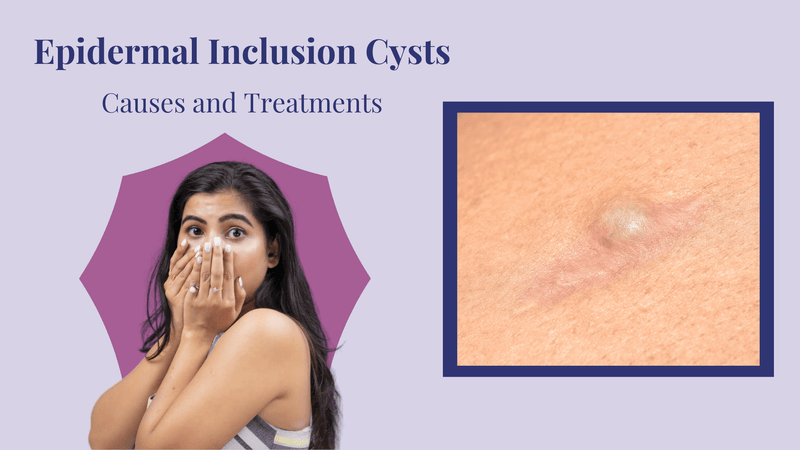
An epidermal inclusion cyst (EIC) is known as an epidermoid cyst, epidermal cyst, or a sebaceous cyst These are all the same thing; a benign hard papule or nodule in the dermis and subcutaneous tissue. It may be also called be called a blind pimple but it is more correct to say EIC.
A sebaceous cyst is the incorrect name for an epidermal inclusion cyst. Years ago it was believed these contained sebum but we now know these are the same as an EIC. (1)
Epidermoid cysts are essentially the same condition as Epidermal Inclusion Cysts (EIC). They are slow-growing lumps that gently push up the skin. One distinct feature many notice is a small, central dot or opening on the cyst, which is known as a "punctum." This punctum is the blocked opening of a hair follicle and its associated oil gland, called the pilosebaceous follicle.
The name difference might be confusing, but whether you hear "Epidermoid cyst" or "EIC," know that they are referring to the same skin condition. Both terms describe benign (non-cancerous) growths that originate from the skin's outermost layer and its associated structures. They're commonly filled with a combination of skin cells and proteins, giving them a cheesy or pasty consistency if ever opened.
How to identify a cyst? Your dermatologist can usually diagnose an EIC by looking at it with a dermatoscope and hearing the history of the bump.
When these are excised, they will be sent to a pathologist if your doctor is concerned about the lesion, because they can be cancer or other skin issues- but this is very rare. The presence of the smelly keratin discharge is a comforting sign of it being benign and not dangerous.
Many things can cause a hard bump or pimple under the skin.
This is the differential diagnosis of what I rule out when I see a hard bump under the skin in my dermatology patients:
Of these, when my patients complain of a blind pimple, they usually have an epidermal inclusion cyst.
Studies are usually not necessary but can be done to diagnose an epidermoid cyst.
When your dermatologist cannot tell if the lesion is a EIC or when it is in a dangerous area such as the midline of the upper face or near large arteries, understanding what's going on under the skin's surface can help the doctor diagnose the cyst. They may turn to imaging techniques like ultrasound and MRI to get a better look.
Let's break down what these tests might reveal if you had an epidermal cyst.
On Ultrasound:
On MRI:
Why This Matters: Understanding these signs is crucial because they help doctors tell the difference between harmless epidermal cysts and potentially harmful growths or tumors (called "neoplastic lesions").
When biopsied or excised and looked at under the microscope, a EIC consists of a cystic space lined by keratinizing squamous epithelium. It is filled with laminated keratinaceous material. The cyst wall is composed of true epidermis with granular layer and contains keratin.
Because it has a true epidermis that makes keratin, an EIC will almost always recur if the epidermal lining (capsule) is not removed.
So if you pop these and extrude the smelly keratin, but you do not remove the lining, the keratin build back up. Think of it as a balloon in the skin that keeps refilling itself.
This is why surgery is the most effective option to remove these.
EICs form when surface epidermis becomes embedded into the dermis from trauma such as picking acne lesions or trying to pop a pimple incorrectly and driving the pus and debris deeper into the skin.
The implanted epidermis continues to proliferate forming a walled off area that secretes keratin, and forms the cystic structure.
The cyst enlarges gradually as more keratin accumulates inside the lumen. The surrounding stroma can develop a foreign body reaction to the leaked keratin.
These cysts often arise from implantation of epidermis following trauma, surgery, or inflammation. They can also develop spontaneously. The slow accumulation of keratin leads to a painless subcutaneous nodule.
Using the right skin care products for your Baumann Skin Type can help prevent getting these cysts on the face.
[[ctaquiz]]
Keratin is the smelly white stuff that comes out of a cyst. It smells bad because of the skin bacteria that uses keratin as a never ending food source. The epidermal lining of sebaceous cysts keeps making more and more of the protein keratin. When the hard bump under your skin gets bigger, this is keratin building up inside the cyst. The thick stinky discharge of acne cysts is what has made the pimple Popper Videos so popular because opening them up can cause a dramatic smelly mess. Most of the pimple popping videos are not pimples but are actually epidermal inclusion cysts.
Cysts last for a long time (months to years) because they do not go away on their own, even if you try to drain it with a needle, draw it out or bring it to a head. How to remove a cyst depends upon where it is located and how large it is. EICS must be surgery removed in most cases. There are several ways to do this. I recommend that you see a dermatologist or plastic surgeon so you have the smallest scar possible. Keep reading to see all the ways to remove or get rid of cysts.
Never attempt to open these EICs yourself because:
PIcking these epidermal cysts or trying to pop them can drive them deeper into the skin and cause scarring. This is a skin problem where you really need to see a dermatologist for treatment. Find one near you here.
Your doctor will do one of the following when you have an epidermal cyst:
Excising the entire cyst is the best way to get rid of it permanently.
You need to be on the right skin care routine for your Baumann Skin Type so that you are not making any of these skin care mistakes that cause cysts:
Using a retinoid such as a retinol is the best way to prevent EICs in most skin types. Here are some retinols that you can begin with, but it is best if you take the quiz so we can tell you all of the products you should use along with the retinol to prevent cysts.
[[ctaquiz]]
[[T11]]
An epidermal cyst will not go away on it's own. You need to get it removed. Once the keratin builds up inside the cyst, it does not get reabsorbed. If you pop the cyst, it will come back. So do not wait for it to go away- see a dermatologist for treatment.
This is keratin made my epidermal skin cells called keratinocytes. It is smelly because of the bacteria that grow and thrives in it.
The bad smell is bacteria. Antibiotics can kill the bacteria and get rid of the smell but you have to take them orally because topical ones cannot get down into the cyst. However, the bacteria will come back. It is better to get the cyst removed than be on antibiotics for a long time just to get rid of the smell.
A black head has an open connection to the skin's surface so it is less likely than a white head to turn into a cyst. But it can turn into a cyst if you improperly squeeze the blackhead. Improperly performed extractions of blackheads commonly cause cysts. This is why you must be very careful extracting blackheads.
Milia and white heads are likely to turn into cysts if you pick them or extract them incorrectly. Pushing on them drives them deep in the dermis which causes an epidermal inclusion cyst.
Cysts do not go away on their own. They may get smaller so you do not see them, but they are still t ere under the skin's surface. They can get infected and grow suddenly. This is why it is a good idea to remove them.
Warm compresses may help bring a cyst to a head. But once you squeeze out the pus, the cyst will return because the capsule has not been removed. So bringing it to a head is not the best way to get rid of a cyst.
You cannot draw out a sebaceous cyst. You can put a topical steroid, injection of a steroid like Kenalog, or anti-inflammatory cream to try to shrink it. But chances are it will come back if not removed by a doctor.
You should try and get on antibiotics within 24 hours if your cyst is infected. It will grow much bigger when infected and the infection can spread to other parts of your skin. See a doctor to make sure you are on the best antibiotic because many skin bacteria are now resistant to common antibiotics.






